During the next phase, the surgeon positions the metal tibial and femoral implants and either cements them to the bone or press-fits them. The next step is to insert a plastic button underneath the kneecap patella. This may require resurfacing the undersurface of the kneecap in order to better affix it to the button. Finally, the surgeon implants a medical grade plastic spacer between the tibial and femoral metal components in order to create a smooth surface that glides easily and mimics the motion of the natural knee.
In order to ensure a successful outcome, the surgeon must align the implants precisely and carefully fit them to the bone. Most are able to resume daily activities. Moderate use of your artificial knee will increase the odds that the implant will last for many years. About 85 to 90 percent of TKR implants continue to work well 15 to 20 years after the operation. Be aware that there are risks are associated with a TKR. These risks include infection that could result in additional surgery, blood clots that could lead to stroke or death, and continued knee instability and pain.
A TKR also requires an extended rehabilitation program and home planning to accommodate the recovery period. You should plan on using a walker, crutches, or a cane immediately after surgery. In addition, implant loosening or failures can occur — especially if misalignment occurred between the implant and the bone during surgery or afterward.
Although these failures are uncommon, and usually occur in the weeks following the original surgery, they would require a return to the operating room for a revision surgery. During this procedure, the surgeon removes the failed implant, once again prepares the bone, and installs a new implant.
There are two different variations of a TKR. Speak to your doctor about which approach is best for you. Removal of the posterior cruciate ligament posterior-stabilized. The posterior cruciate ligament is a large ligament in the back of the knee that provides support when the knee bends.
In this Article:
In its place, special implant components a cam and post are used to stabilize the knee and provide flexion. Preservation of the posterior cruciate ligament cruciate-retaining. If the ligament can support an artificial knee, the surgeon may leave the posterior cruciate ligament in place when implanting the prosthesis. Preserving the cruciate ligament is thought to allow for more natural flexion. Partial knee replacement PKR , sometimes referred to as a uni-compartmental knee replacement, is an option for a small percentage of people.
As the name implies, only a part of the knee is replaced in order to preserve as much original healthy bone and soft tissue as possible. Candidates for this type of surgery generally have osteoarthritis in only one compartment of their knee. So surgery takes place in any of three anatomical compartments of the knee where diseased bone presents the most pain: During a PKR, a surgeon removes the arthritic portion of the knee — including bone and cartilage — and replaces that compartment with metal and plastic components.
A PKR surgery offers a few key advantages, including a shorter hospital stay, faster recovery and rehabilitation period, less pain following surgery, and less trauma and blood loss. Compared with those who receive a TKR, people who receive a PKR often report that their knee bends better and feels more natural. Surgeons usually perform PKRs on younger patients under age 65 who have plenty of healthy bone remaining. The procedure is performed on one of the three knee compartments.
Knee Surgeries Could Soon Be More Successful Thanks to New Technique
PKRs are most suitable for those who lead an active lifestyle and might require a follow-up procedure — perhaps a TKR — in 20 years or so, after the first implant wears out. Because a PKR is less invasive and involves less tissue, you are likely to be up and about sooner.
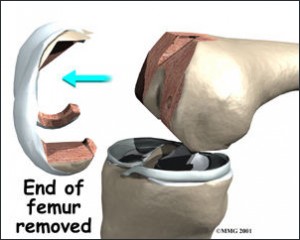
In many cases, a PKR recipient is able to move around without the aid of crutches or a cane in about four to six weeks — approximately half the time for a TKR. They also experience less pain and better functionality — and report high levels of satisfaction. Next, specialized alignment rods and cutting jigs are used to remove enough bone from the end of the femur thigh bone , the top of the tibia shin bone , and the underside of the patella kneecap to allow placement of the joint replacement implants. Proper sizing and alignment of the implants, as well as balancing of the knee ligaments, all are critical for normal post-operative function and good pain relief.
Again, these steps are complex and considerable experience in total knee replacement is required in order to make sure they are done reliably, case after case. Provisional trial implant components are placed without bone cement to make sure they fit well against the bones and are well aligned.
At this time, good function--including full flexion bend , extension straightening , and ligament balance--is verified. Finally, the bone is cleaned using saline solution and the joint replacement components are cemented into place using polymethylmethacrylate bone cement. The surgical incision is closed using stitches and staples. Total knee replacement may be performed under epidural, spinal, or general anesthesia. We usually prefer epidural anesthesia since a good epidural can provide up to 48 hours of post-operative pain relief and allow faster more comfortable progress in physical therapy.
No two knee replacements are alike and there is some variability in operative times. A typical total knee replacement takes about 80 minutes to perform. Whenever possible we use an epidural catheter a very thin flexible tube placed into the lower back at the time of surgery to manage post-operative discomfort.
Latest Knee Surgery Techniques | Knee Surgeon Miranda NSW | Sydney
This device is similar to the one that is used to help women deliver babies more comfortably. As long as the epidural is providing good pain control we leave it in place for two days after surgery. After the epidural is removed pain pills usually provide satisfactory pain control. Patients with a good epidural can expect to walk with crutches or a walker and to take the knee through a near-full range of motion starting on the day after surgery.
Following discharge from the hospital most patients will take oral pain medications--usually Percocet Vicoden or Tylenol for one to three weeks after the procedure mainly to help with physical therapy and home exercises for the knee. Aggressive rehabilitation is desirable following this procedure and a high level of patient motivation is important in order to get the best possible result.
Oral pain medications help this process in the weeks following the surgery. Most patients take some narcotic pain medication for between 2 and 6 weeks after surgery. Patients should not drive while taking these kinds of medications. While any surgical procedure is associated with post-operative discomfort most patients who have had the total knee replacements say that the pain is very manageable with the pain medications and the large majority look back on the experience and find that the pain relief given by knee replacement is well worth the discomfort that follows this kind of surgery.
You are here
Physical therapy is started on the day of surgery in the hospital or the very next day after the operation. Patients are encouraged to walk and to bear as much weight on the leg as they are comfortable doing. Range-of-motion exercises are initiated on the day of surgery or the next morning. The physical therapist should be an integral member of the health care team. The average hospital stay after total knee replacement is three days and most patients spend several more days in an inpatient rehabilitation facility. Patients who prefer not to have inpatient rehabilitation may spend an extra day or two in the hospital before discharge to home.
We recommend inpatient rehabilitation for most patients to assist them with recovery from surgery. The average stay in a rehab unit is about 5 days. This is especially important for older patients and individuals who live alone. These arrangements are made prior to hospital discharge.
Patients are encouraged to walk as normally as possible immediately following total knee replacements. Most people use crutches or a walker for several weeks to a month following total knee replacements and then a cane for a couple of weeks beyond that. Patients should not resume driving until they feel their reflexes are completely normal and until they feel they can manipulate the control pedals of the vehicle without guarding from knee discomfort. Certainly patients should not drive while taking narcotic-based pain medications. On average patients are able to drive between three and six weeks after the surgery.
Following hospital discharge or discharge from inpatient rehabilitation patients who undergo total knee replacement will participate in either home physical therapy or outpatient physical therapy at a location close to home.
- A Treatise on the Soul?
- Franco (Text Only): A Biography;
- Partial knee replacement!
- ?
- Dragonkin: A Tor.Com Original!
The length of physical therapy varies based upon patient age fitness and level of motivation but usually lasts for about six to eight weeks. Two to three therapy sessions per week are average for this procedure. At first physical therapy includes range-of-motion exercises and gait training supervised walking with an assistive device like a cane crutches or walker. As those things become second nature strengthening exercises and transition to normal walking without assistive devices are encouraged.
All patients are given a set of home exercises to do between supervised physical therapy sessions and the home exercises make up an important part of the recovery process. However, supervised therapy--which is best done in an outpatient physical therapy studio--is extremely helpful and those patients who are able to attend outpatient therapy are encouraged to do so. For patients who are unable to attend outpatient physical therapy, home physical therapy is arranged.
Most people walk using crutches or a walker for weeks then use a cane for about more weeks. Sometime between one and two months post-operatively most, patients are able to walk without assistive devices. Most patients obtain and keep at least 90 degrees of motion bending the knee to a right angle by the second week after surgery and most patients ultimately get more than degrees of knee motion.
Most patients can return to sedentary desk jobs by about weeks; return to more physical types of employment must be addressed on a case-by-case basis. Most patients are back to full activities--without the pain they had before surgery--by about three months after the operation. The goal of total knee replacement is to return patients to a high level of function without knee pain. The large majority of patients are able to achieve this goal. However, since the joint replacement components have no capacity to heal damage from injury sustained after surgery we offer some common-sense guidelines for athletic leisure and workplace activities:.
Since the joint replacement includes a bearing surface which potentially can wear, walking or running for fitness are not recommended. Some patients feel well enough to do this and so need to exercise judgment in order to prolong the life-span of the implant materials. Swimming, water exercises, cycling, and cross country skiing and machines simulating it, like Nordic Track can provide a high level of cardiovascular and muscular fitness without excessive wear on the prosthetic joint materials.
Total knee replacement is a reliable surgical technique in which the painful arthritic surfaces of the knee joint are replaced with well-engineered bearing surfaces. Like any major procedure there are risks to total knee surgery and the decision to have a knee replacement must be considered a quality-of-life choice that individual patients make with a good understanding of what those risks are. Knee replacement is a surgical technique that has many variables. Like most areas of medicine, ongoing research will continue to help the technique evolve. It is important to learn as much as possible about the condition and the treatment options that are available before deciding whether--or how--to have a knee replacement done.
Overview Symptoms Diagonsis Treatment Surgery Physical Therapy Summary Overview This article reviews the benefits, risks, and alternatives to total knee replacement surgery which is sometimes called total knee arthroplasty. Broadly speaking there are two types of knee replacements: Partial Knee Replacement Partial knee replacements have been around for decades and offer excellent clinical results, just like total knee replacements.
Patient Success Video In the video below a patient is skiing deep powder at Bridger Bowl Montana on a total knee replacement. Please note, not all patients are able to ski and we do not recommend this activity to patients with knee replacements Symptoms Characteristics of severe arthritis of the knee Pain Pain is the most noticeable symptom of knee arthritis.
Stiffness Morning stiffness is present in certain types of arthritis. Swelling and warmth Patients with arthritis sometimes will notice swelling and warmth of the knee. Medial-sided knee pain, located on inside part the knee, is the most common location for arthritic pain. Isolated patellofemoral arthritis is the least common pattern of knee arthritis. This patient was later treated with a total knee replacement similar to the one shown in Fig. The results are OK, but people are always looking to possibly improve on it.
ACI has been proven to provide long-lasting pain relief and to help patients regain knee function. Most of our work is with microfracture. MACI was not yet available in the U. We received FDA approval for it in December and launched it in early Once you have those injuries, the cartilage is not going to repair itself. In some cases, osteochondral allografts, or OCAs, are performed. These are bone and cartilage grafts sourced from cadavers instead of the patient.
But the supply of grafts is limited and the procedure is highly invasive. In addition, controlled clinical trials have not been run, since tissue bank products are subject to a lower level of regulation. Some physicians believe the procedure has a higher risk of failure. The only option to regrow your own cartilage is ACI.
- Le guide des vins de Bordeaux (Documents Français) (French Edition).
- Total knee replacement!
- Mármara (Spanish Edition).
- related stories.
- Extreme Birder: One Womans Big Year.
- Origine du nom de famille LONGUET (French Edition);
- ?
Once the doctor is satisfied with the fit, the MACI membrane is glued into place. The cells migrate onto the bone, adhere to it, start to replicate, and initiate cartilage production to fill in the defect. The FDA has approved MACI for first-line treatment of any cartilage defects of the knee, but not for the meniscus the thin fibrous cartilage between the surfaces of the knee , Michel said. One California team physician who uses MACI has achieved gratifying results with some of his patients, who include college and professional athletes.
Patients can expect to return to pain-free simple activities of daily living within four to six months.
