A view, therefore, began to gain currency that the government needed to intervene either to require that everybody buy such insurance or to use some of its tax resources to do this for the poor instead of handing over the amount to them as direct cash benefit transfers. However, while this does address some of the problems, it does not by itself result in a good health system design without the benefit of several other complementary interventions which change the manner in which healthcare is purchased and how providers are paid.
For that to happen, the price has to be set at or near the cost of production. Unfortunately, asymmetry of information between providers and patients give providers significant monopoly power, if left unregulated, to set prices way above cost. Further, providers have the ability to influence patient preferences by recommending them more quantity and more intensive treatment than clinically justified supplier induced demand , leading to waste and inefficiency, and ultimately, they are paid for by the patients.
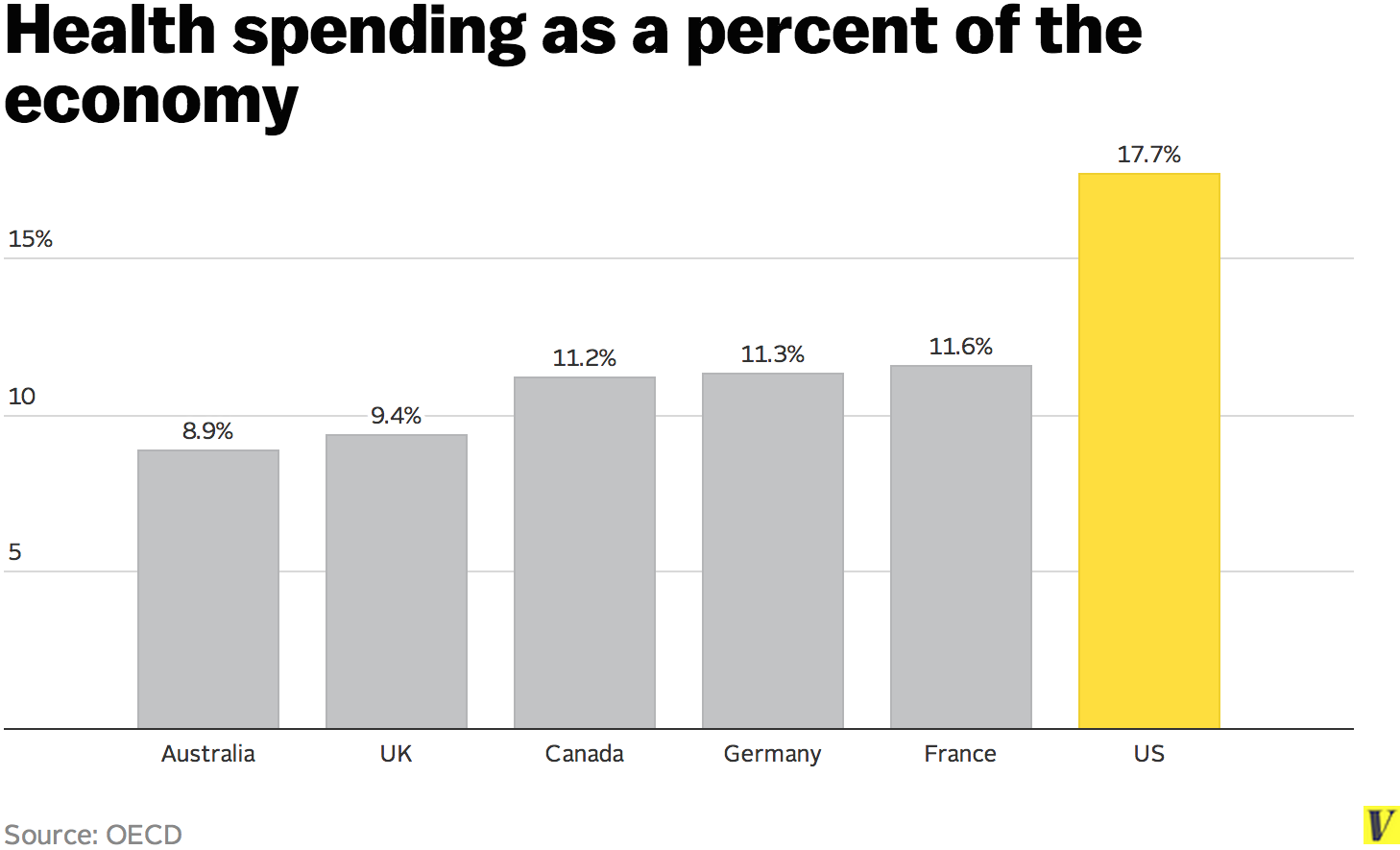
Governments have every role and responsibility to set the right price for both providers and consumers in these situations. Given all of these features of healthcare, it is now clear to all countries, including almost entirely free-market based economies such as the US, that policymaking based on a simplistic understanding of the role of the government and that of the functioning of markets is likely to lead countries seriously astray and result in equilibria that are neither efficient nor welfare maximizing.
However, it is not the case that the only alternatives to market fundamentalism are full financing of the healthcare system from general tax revenues or the full provision of all healthcare by the government. Each country and, for large countries like India and China, each region within a country, would have to carefully think through its unique situation and find answers to these complex questions in a manner that best suits its environment, culture and resources.
It is gratifying to observe that countries as different as the Philippines, Ghana, Thailand, Indonesia, Kenya and Kazakhstan have started down this journey and are in the process of putting in place the pillars of a sound health system, which combine the role of the government and the free market in a thoughtful way.
Price Transparency in Health Care: Highlights from the Task Force Report
A surgery nurse puts on gloves before procedures on a patient. The views expressed in this article are those of the author alone and not the World Economic Forum. The link between migration and technology is not what you think Marie McAuliffe 14 Dec Politics is failing to protect the Amazon. More on the agenda. Faced with a rising tide of bad debt, a large Southeastern healthcare system was seeing a sharp decline in net patient revenues.
The need to improve collections was dire. By integrating critical tools and processes, the health system was able to increase online payments and improve its financial position. This case study explains how. With the ICD10 deadline quickly approaching and daily responsibilities not slowing down, final preparations for October 1 require strategic prioritization and laser focus.
Read how Gwinnett Medical Center provides clear connections to financial information, offers multiple payment options for patients, and gives onsite staff the ability to collect payments at multiple points throughout the care process. To maintain fiscal fitness and boost patient satisfaction and loyalty, healthcare providers need visibility into when and how much they will be paid—by whom—and the ability to better navigate obstacles to payment.
They need payment clarity. This whitepaper illuminates this concept that is winning fans at forward-thinking hospitals.
Price Transparency in Health Care: Highlights from the Task Force Report | HFMA
Financial services staff are always looking for ways to improve the verification, billing and collections processes, and Munson Healthcare is no different. Effective revenue cycle management can be a challenge for any hospital, but for smaller providers it is even tougher. Read how Wallace Thomson identified unreimbursed procedures, streamlined claims management, and improved its ability to determine charity eligibility. Healthcare leaders should consider taking the steps outlined in the whitepaper to ease the process of gaining approval, piloting, implementing, and supporting sustainability projects.
You will find that investing in sustainability and energy efficiency helps hospitals add cash to their bottom line. Discover how hospitals and health systems have various options for funding energy-efficient and renewable-energy initiatives, depending on their current financial structure and strategy. Health care is a dynamic mergers and acquisitions market with numerous hospitals and health systems contemplating or pursuing formal arrangements with other entities.
These relationships often pose a strategic benefit, such as enhancing competencies across the continuum, facilitating economies of scale, or giving the participants a competitive advantage in a crowded market. Underpinning any profitable acquisition is a robust capital planning strategy that ensures an organization reserves sufficient funds and efficiently onboards partners that advance the enterprise mission and values. This whitepaper offers several strategies that health system leaders have used to assess and manage capital needs for their growing networks.
Announcements from several commercial payers and the Centers for Medicare and Medicaid Services CMS early in around increased efforts to form value-based contracts with providers seemed to point to an impending rise in risk-based contracting. Rather than wait for disruption from the outside in, health care providers are now making inroads on collaborating with payers on various risk-based contracting models to increase the value of health care from within.
Before becoming a ZirMed client, Yuma was attempting to manually monitor hundreds of thousands of charges which led to significant charge capture leakage.
The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary.
Every facility and challenge is unique, and requires a full objective analysis. As the critical link between patient care and reimbursement, health information enables more complete and accurate revenue capture. Speedier cash flow starts with better CDI and coding.
- TRÖDEL NICHT, ADAM (German Edition).
- Lena River Man.
- INTRODUCTION.
This 5-Minute White Paper Briefing explains how providers can improve vital measures of technical and business performance to accelerate cash flow. Qualified coders are getting harder to come by, and even the most seasoned professional can struggle with the complexity of ICD This 5-Minute White Paper Briefing explains how partnerships can help improve coding and other key RCM operations potentially at a cost savings.
The reasons claims are denied are so varied that managing denials can feel like chasing a thousand different tails. Read about how predictive modeling can detect meaningful correlations across claims denials data. Emergency Mobile Health Care EMHC was founded to be and remains an exclusively locally owned and operated emergency medical service organization; today EMHC serves a population of more than a million people in and around Memphis, answering 75, calls each year.
Included in this whitepaper are implications of increasing patient responsibility, collections best practices, and collections and internal control solutions. Yet even for the best billers, achieving that success can be elusive when denials stand in the way of success, presenting challenges at every turn. Join practice management expert Elizabeth W. Discover methods to translate denial data into business intelligence to improve your bottom line, determine staff productivity benchmarks for billers, and recognize common mistakes in denial management. Physician practices must improve organizational efficiency to compete in this era of reduced reimbursement and escalating administrative costs.
Many healthcare organizations are pursuing next-generation health information systems solutions. As value-based payment models evolve, providers are challenged to maintain superior clinical outcomes while controlling costs. Read more about factors contributing to the changes in the post-acute marketplace and what it means for manufacturers, physicians, clinicians, patients, and post-acute facilities as they anticipate the transition to the second curve. HSG helped the physicians and executives of St. Income can influence demand for healthcare. If a consumer is a low-income earner, the consumer may not seek healthcare for common sickness.
Likewise, a consumer who earns more may be more willing to spend on healthcare. Policies such as subsidy can increase demand for healthcare as patients are charged a lower price. Is a fundamental concept in economics that describes the total number of a specific good or service available to consumers. Supply can be determined by price, competing goods, and demand [ 1 ]. Healthcare is different from other services because it is not clearly defined. In most industries, the product or service can be standardized to improve efficiency and quality.
In healthcare, every consumer is structurally, chemically, and emotionally different. What works for one person may not necessarily work for another. Healthcare also differs in terms of choosing consumers. In other services, there is a choice in selecting which person or industry business can be conducted with. Furthermore, healthcare professionals are rarely paid directly by their patients like in other industries. Payment usually comes from government or insurance companies.
These factors make healthcare unique when compared with other services. The demand for healthcare comes from the desire of the consumer to gain good health. Most people prefer being healthy to being sick. Another factor that makes health care different from most other goods and services is that it is simultaneously an investment. The money consumer spends on being healthy today will also benefit the consumer in the future. Another key characteristic of health care is that demand is relatively inelastic [ 5 ].
Joe Fifer on improving price transparency
If a consumer is sick and requires medical care, the consumer will purchase healthcare services at almost any price. Unlike other goods or services, the quality of health makes it difficult to meet the ideal market solution. Health is not a marketable product.
For instance, Customer A cannot change his or her hemoglobin A1C result of 5. In other services, if Mr. A purchases an air purifier online from Amazon, if he chooses to return the product because of any reason, he can. If he decides he wants to sell it on Craigslist, he can also do that. This type of exchange is not possible when it comes to health. According to Mwachofi and Al-Assaf [ 3 ], with other services, demand can be predictable, and consumers have the ability to test the product or service before consumption.
- Viewing options.
- What role should governments play in healthcare? | World Economic Forum.
- Share This Article?
- The Story of Percy;
- The Last Fruit. Stories from Laos.
For instance, If Mr. G a 30 days free and no commitment trial period. This type of service is not possible in healthcare. A patient cannot have a 30 days trial for gastric bypass.