To meet the long-term care needs of Baby Boomers, social and public policy changes must begin soon. Meeting the financial and social service burdens of growing numbers of elders will not be a daunting task if necessary changes are made now rather than when Baby Boomers actually need long-term care. A major public policy concern in the long-term care field is the potential burden an aging society will place on the care-giving system and public finances. This paper assesses the economic dimensions of the problem.
The first half of the paper reviews the literature and logic that suggest that aging in general, and long-term care services in particular, will represent an overwhelming economic burden on society by Then, a new analysis of burden is presented to suggest that aggregate resources should not be a major issue for the midcentury economy. Finally, the paper presents four key challenges that represent the real economic burden of long-term care in the twenty-first century.
These challenges are significant but different from macro cost issues. What type of economic burden might be considered overwhelming? Existing literature never explicitly defines this but the sense is that the burden might be considered overwhelming if: The discussion has significant implications for public policy and for private actors focused on developing an effective care system for the mid—twenty-first century. Public policy goals related to an aging society must balance the need to provide adequate services and transfers with an interest in maintaining the economic and social well-being of the nonelderly.
The economic challengesdiscussed are such that public and private progress that begins in the near future will make the future burden substantially easier to handle. Various aspects of economic burden are associated with an aging population: Much of the logic of the paper applies to each of these financial resource challenges. However, we focus principally on the implications of long-term care services, which along with prescription drugs, have had the fastest growing costs in the list cited. In most other countries, these items tend to be financed socially. Estimates calculated by authors.
See footnote 1 for assumptions used.
Long-term care includes a broad continuum of services that address the needs of people who are frail or disabled and require help with the basic activities of everyday living. The services can vary from informal care delivered by family and friends to the formal services of home care, assisted living, or nursing homes see Table 2. Long-term care professionals generally distinguish two types of supportive care needs for the frail: These statistics measure the number of elderly who are disabled at any given point in time.
Most elderly who live beyond 75 or 85 years of age become frail at some point and need some form of assistance, making lifetime risks much higher. In fact, 42 percent of people who live to the age of seventy will spend time in a nursing home before they die Murtaugh et al. When resources expand, new services develop quickly, and when resources contract, capacity can also shrink quickly.
In home health care, for example, annual expenditure growth rates went from more than 10 percent in the s and early s to minus 3 percent between and Levit et al. Recent policy revisions including the Home Health Prospective Payment System and the Balanced Budget Refinement Act, along with projected strong growth in out-of-pocket spending by individuals and families, cause many analysts to believe that home health care spending will rise again in the coming decade Heffler et al. Of course, expansion and contraction of nursing home beds respond more slowly to market forces because of the durable capital aspect of nursing home care.
Out-of-pocket expenses account for almost all of the balance, with private insurance covering just 1 percent of long-term care costs See Figure 1. Conservative CBO estimates suggest total long-term care expenditures will increase at a rate of 2. The numbers are slightly different if one assumes that long-term care insurance does not become more common, but the stark upward trend remains. Among the elderly who require assistance with daily activities, 65 percent rely exclusively on families and friends and another 30 percent rely, at least in part, on informal care.
The argument that caring for an aging society could disable the American economy has been made by various commentators, perhaps most forcefully by Peter Peterson and others in the Concord Coalition Peterson Their concern focuses on the large growth in the number of elderly over the coming years, from 35 million in to more than 80 million in Figure 2.
By Andrew Wister
This growth in elderly could lead to a precipitous drop in the number of workers per elderly if current working and retirement patterns do not change Figure 3. Thus, the ratio of workers to frail elderly could decrease even more dramatically than the ratio of workers to all elderly. A second part of the argument that long-term care could be a large burden focuses on the rapid inflation in expenditures for long-term care in recent years.
These increases have not been offset by lower out-of-pocket payments, although growth rates for the latter have been lower and more consistent, with average increases of 7 percent for home health care and 3. Finally, many professionals believe that even at current expenditure levels, there is a significant amount of unmet need for long-term care among the frail, and no foreseeable end in upward pressure on per diem service costs Allen and Mor A final part of the argument for concern about long-term care costs comes from unsettling survey results reported by Curran, McLanahan, and Knab in review suggesting that children who experience divorce may be less willing or able to care for their aging parents.
Their data indicate that the probability of an elderly person perceiving an availability of emotional support from his or her children is reduced from 71 percent for those who marry once and remain married to 56 percent for those who marry and divorce. Remarrying after divorce provides some additional support, but does not completely offset the result of the first divorce. With the legacies of the divorce boom getting older, the percent of the elderly who are divorced or separated is projected to double for men and triple for women between now and It may be the case that informal care resources will shrink and thus result in even more pressure on public and private resources that support the formal care system.
It is possible to construct a counter-case that is more optimistic about the macro burden of long-term care in the twenty-first century. Most importantly, the typical analysis of dependency ratios overstates the impacts of aging on burden. While standard calculations include only the to year-old population as producers, and places all of the and-older population in the dependency group because of eligibility for Social Security and Medicare , this approach is not appropriate in the case of long-term care.
At the very least, the denominator should include only people 75 and older since the to year-old age group does not use large amounts of long-term care. The percentage of elderly older than 85 years who are ADL impaired or institutionalized is more than six times the rate of to year-olds Manton, Corder, and Stallard In fact, if the Baby Boom generation is healthier than past generations as argued later in the paper , it very well could be that the young elderly might work longer and thus be considered producers.
In addition, in considering macroeconomic burden, the other group of dependents in society—children—should be included in the denominator with the elderly, as both groups are dependent on the adult population. Recalculating dependency ratios using these new principles see Table 4 indicates improvements rather than deteriorations in the adult to dependency ratios, especially when the year is compared to when children were present in the population in peak numbers.
When to year-olds are compared to children and individuals 75 or older, the dependency ratio actually improves between and All of these ratios change in unfavorable directions between and , but the changes are not substantial. A second factor that might make the burden of long-term care less striking than expected in is improvement in the health status of the elderly. Recent data from the National Long-Term Care Survey reported by Manton and Gu indicates that the disability rate for all elderly dropped from This meant that there were more than , fewer disabled elderly in than in , despite a one-third increase in the population of the elderly.
In prior work, Singer and Manton estimated that a relative rate of disability decline of 1. This decline is actually significantly less than the 2. Declines in the nursing home population, particularly among the oldest old, have accompanied these disability trends Bishop A more mixed, although guardedly optimistic, picture of disability trends has been offered by other demographers Crimmins ; Reynolds et al.
However, they caution that this decline was not persistent or consistent through this period, with most of the decline occurring in the s. Although trends will need to be watched closely over the coming decades, declines in disability probably will continue. The elderly of will be much better educated, with a college graduation rate twice and high school drop out rate one-third that of the current generation of elderly U. Department of Education This bodes well for the future physical health of aging Baby Boomers, as there is a strong correlation between education level and disability; college graduates have a disability rate about half that of high school dropouts.
Expected advances in medicine, through prevention, pharmaceuticals, and surgical treatments, should also reduce the need for long-term care. More and more older patients are benefiting from restorative treatments, such as knee replacements and coronary angioplasty, once unavailable due to age Lubitz et al. Although such advances in medicine tend to increase acute health care costs, these treatments can delay entrance into nursing homes and other long-term care needs.
Better pharmaceuticals for preventing and treating disabling conditions such as osteoporosis, arthritis, and rheumatism will continue to decrease the number of elderly who need assistance with IADLs and ADLs Neer et al. Because about 60 to 70 percent of nursing home residents have dementia-related symptoms Rovner and Katz , progress in treating or preventing Alzheimer's and other dementias associated with later life could lead to large reductions in the number of elderly with the most intensive long-term care needs. This is already happening: Freedman, Aykan, and Martin found that the proportion of noninstitutionalized elderly—particularly the very elderly—with severe cognitive impairment between and fell from 6.
If as a result of further medical advances and social shifts, the disability rates continue to decline in the coming years at the same pace that Manton reported for to , or an average 0. This seems extremely unlikely. A more conservative estimate for declines in disability rates would be an average annual decline of 0. Although this decline would be half the 0. Even a moderate decline in disability would have dramatic impacts on the economic burden of long-term care. The optimistic forecasts could be affected by demographic changes that are difficult to forecast.
Most relevant perhaps are trends in immigration. It is possible that unexpected growth in immigration could increase the number of elderly in the year , making burdens worse. Or, immigration trends might also bring larger than expected numbers of working-age adults to America, thus decreasing dependency ratios. In addition, Wolf makes the case that decreases in disability rates that are due to higher educational attainments among the Baby Boom generation will not continue past the year The final and most important factor that will affect the macro burden of aging is the future of the American economy.
When the pessimistic literature on the burden of an aging society was published, the economy was growing at anemic rates and inflation rates were relatively high. If the economy grows at a steady, healthy pace, the overall burden of long-term care will be moderate. Social security actuaries issue three different economic scenarios for the coming century. During the s, a decade when yearly change in real GDP shifted from negative numbers to above 4 percent, GDP actually averaged about 3 percent real annual growth per year.
The Problem: Caring for Aging Baby Boomers
If GDP growth were to continue at 3 percent over the next three decades, a rate which few believe is possible, LTC expenditures as a percentage of GDP would actually decline between and Whether real GDP growth averages 1, 2, or 3 percent will make an enormous difference over a thirty-year timeframe. Taken together, these three factors—newly calculated dependency ratios, declines in disability rates, and healthy economic growth—could work together to make the macro burden of long-term care no worse than it is the beginning of the twenty-first century.
While the future remains uncertain, there seems to be little reason for dire concerns about the future burden of long-term care. Our estimates are meant to be broad outlines rather than specific forecasting. Others have eloquently discussed the power of and caveats to making demographic and economic projections Lee and Skinner Despite the preceding positive analysis of the macroeconomics of aging, there remain some substantial challenges to getting ready to meet the long-term care needs of Baby Boomers.
In fact, four types of challenges need to be addressed:. Each of these challenges is considered in the remaining sections of this paper. Four sources of payments currently finance long-term care services for the elderly: Medicare, Medicaid, private insurance, and out-of-pocket payments see Figure 4. The federal Medicare program pays for approximately 24 percent of all long-term care costs Congressional Budget Office Medicare's long-term coverage, however, focuses mostly on home care that is related to medical problems, such as broken hips.
Services generally are restricted to people receiving rehabilitation for some medical condition. In principle, Medicare does not cover custodial long-term care, but in practice it is an ongoing challenge for Medicare and providers to distinguish custodial care and rehabilitative care. Medicaid acts as a backstop, paying for long-term care services for the frailest elders when they are poor.
In most states, the Medicaid program pays for care for the poor and for elders who become poor when long-term care expenses impoverish them. In , 64 percent of elderly nursing home residents used Medicaid to finance at least some of their care Dey In many states, a large share of all Medicaid long-term care dollars supports frail elders who had been middle class before becoming frail. In New York State, for example, the Medicaid program pays for 80 percent of all nursing home costs; clearly, 80 percent of New York elders are not poor before they become frail.
Most states direct the lion's share of Medicaid dollars to nursing homes as opposed to home care. In , almost 85 percent of elderly Medicaid long-term care expenditures were for institutional care and only 10 percent were for home care services Wiener and Stevenson This is a result of Medicaid's attempts to focus on the most frail, who tend to be in nursing homes.
Many experts feel that this emphasis on nursing homes means that not enough resources are devoted to preventing elders who have some disabilities from becoming more and more frail Kane, Kane, and Ladd Since elders tend to avoid nursing homes as long as possible, the Medicaid emphasis on nursing homes means that many elders go without community-based services that really could help them live better lives.
Private insurance accounts for just 4 percent of long-term care costs. Despite aggressive attempts by the insurance industry to develop a private market for long-term care, the growth of this market has proceeded slowly. Part of the reason is the nature of the contract between an insurer and an elder. The insurer needs to guarantee a service that often will occur twenty or more years after the contract is set.
The 2030 Problem: Caring for Aging Baby Boomers
The uncertainty leads insurers to keep prices high and makes elders nervous about purchasing a private insurance policy. And, the reluctance of people to think about purchasing such insurance at younger ages makes the payments on an insurance policy beyond the reach of many elders. Finally, the availability of Medicaid as a substitute for private insurance leads many elders to forego insurance premiums and take their chances on remaining healthy McCall etal. Out-of-pocket costs finance about 36 percent of long-term care, but the burden of these payments is very unevenly distributed.
The 42 percent of elders who spend some time in a nursing home—one-half of them for two years or more—pay most out-of-pocket costs for long-term care. Why is it so hard to devise a financing system to replace the current patchwork payment approach? It is very difficult to judge who really needs formal long-term care services, and there may be large amounts of pent up demand currently taken care of by families and friends.
The woodwork effect predicts that total expenditures could grow substantially if public and or private insurance expanded Weissert, Cready, and Pawelak ; Kane, Kane, and Ladd Imbedded within the woodwork issue is the real social challenge of determining how best to allocate limited resources. Any expanded public insurance system would require new taxes.
And private insurance would be paid for from private savings, which are in short supply for most middle-income elders. One interpretation of the indifference of working-age Americans to either save privately or approve taxes to cover future long-term care services is that Americans are not adequately aware of the implications of these nonactions. Perhaps Americans, more so than other societies, are less mindful of the needs of aging due to a relatively age-stratified society.
The other interpretation, however, is that Americans do not value long-term care services. This interpretation is bolstered by the fact that many moderate-income elderly who could benefit from long-term care and could afford to pay for some services choose to make do on their own. In addition, financing reform has had to compete with various other social priorities. In recent years, lawmakers have directed more attention toward uncovered pharmaceutical costs. Medical care costs in general are high for elders—even with Medicare, elders and their families pay more than a third of their health care costs out of their own pockets.
The large number of uninsured among the nonelderly population continues to be a problem that demands attention. The needs of elders also compete for resources with other problems facing other age groups. Many have concluded that elders have done rather well with social policy compared with other needy subgroups of our population. Child poverty, for example, is higher today than it was three decades ago, while poverty among the elderly has decreased significantly.
Finally, tax cuts and a sluggish economy could completely eliminate the funds needed for any new social programs. Any specific person who becomes frail may face higher burdens because the expected value averages high costs for those who become frail and zero costs for those elders who avoid the need for long-term care services. And, home care costs can be just as high for a frail elder wanting to live at home. Medicaid Bound, Financially Independent, and Tweeners. These are individuals who have few financial resources available for long-term care and who have no choice but to rely on Medicaid.
This is a group whose lifetime income and wealth are adequate but who cannot handle a long-term care shock. Estimates calculated using the Lewin Long-Term Care Financing Model indicate some good news about the future financial viability of elders. In the year , an estimated 45 percent of elders are classified as Medicaid Bound but this estimated percentage drops to 29 percent in the year By contrast, the share of the elderly who are financially independent increases from 27 percent in to 38 percent in As with all simulations and forecasts, the estimates into the future depend on key economic assumptions.
The assumptions used follow the principles of the middle estimates of the social security forecasting model: To meet this forecast, long-term care cost inflation would need to be brought under control. If long-term care costs increase at 2. Thus, a relatively modest increase in long-term care inflation rates could eliminate the rosy simulation estimates of changes in the Medicaid Bound as reported above.
The other interesting forecast that emerges from the simulation exercise is that the percentage of people in the Tweeners category will not shrink, but will actually increase from 28 percent to 33 percent. This implies that there will continue to be a large number of middle class elderly who will spend down to Medicaid coverage unless new financing arrangements help make the Tweeners more self-reliant.
How do assumptions about future disability rates affect the simulation results? In fact, disability rates only affect the estimates indirectly in that higher disability rates lead to lower income and asset estimates—particularly for the nonelderly—and this increases the number of Medicaid Bound. Disability rates do not directly affect the simulation estimates because the calculations assess who is able to afford long-term care at a point in time whether a person is disabled or not. Despite the size of the economic shock associated with long-term care needs, very little policy attention is being given to designing new approaches to pay for long-term care.
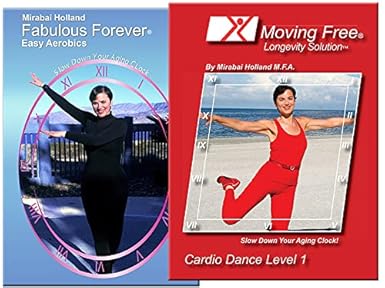
Product details
The Kaiser Family Foundation issued a side-by-side comparison of key health policy positions advanced by the Gore campaign and the Bush campaign in early October The quiet long-term care issue for the elderly was completely eclipsed by attention to prescription drug coverage and the future of social security during the presidential campaign.
When attention does focus on financing options for long-term care, three serious types of options need to be considered: Tax deductibility for private insurance premiums clearly would expand the number of people who purchase long-term care insurance. Deductibility would lower the after tax cost of insurance by 15 percent to 40 percent the range of the current marginal tax rates.
Unfortunately, the largest after-tax price breaks would go to the most wealthy people who do not need insurance because they can afford to pay for long-term care from existing resources. Thevast majority of working age, middle-class people—who comprise the Tweeners—would experience between a 15 and 25 percent reduction in the costs of insurance premiums after tax deductibility. While this would be a welcome incentive, past experience with lowering the marginal cost of insurance for middle class families suggests that most will not begin to purchase long-term care insurance unless a major portion of the premium is paid for.
Bilheimer and Colby The most likely option for a public program for insuring long-term care would involve a voluntary-type program based on out-of-pocket payments for premiums similar to Part B of Medicare. This type of program could offer graduated subsidies to make long-term care insurance more affordable for moderate-income people. In order to make the insurance affordable for most people, however, the subsidies would probably need to be large. While this type of program should lead to substantial reductions in Medicaid payments for Tweeners, the net public sector costs would likely be substantial.
Public offerings of insurance would avoid many of the marketing problems associated with private long-term care insurance and would create some healthy competition between existing private insurance policies and the new public offering. A public long-term insurance program with targeted subsidies would likely cause a much bigger expansion of insurance for middle-class families than would occur in a comparably scaled, tax deductibility program.
The third type of financing improvement would follow the logic of advocates for privatizing social security: Mandatory savings in private investment accounts could be required for all individuals starting at an age that would make annual savings affordable. Deborah Lucas presents a detailed plan for a mandatory savings approach to private financing. However, the estimated savings rate for prefunding starting at age 55 is almost four times that of prefunding starting at age 35 and would also be quite sensitive to interest rates Lucas More analysis of these options—and others that might emerge—is needed to encourage some consensus about how to improve the financing of long-term care for the Medicaid Bound and Tweeners.
A few important principles that should guide reform debates emerge from the analysis presented here:. Perhaps consensus about which option is the best reform approach for long-term care financing can emerge only if there is consensus about the criteria for judging options.
Unfortunately, the criteria tend to conflict with one another, forcing stark trade-offs. For example, one desirable criterion for assessing options is the extent to which individuals have free choice to select a method of preparing for their possible long-term care needs. Options strong on this criterion tend to be weak on another desirable criterion: A third criterion also may conflict with the other two desirable features: At the very least, debates about options need to make clear what criteria related to effectiveness are under consideration.
While the Baby Boomers were growing up, the needs of young families were a high priority in community development, with particular concern for family-friendly housing, parks, and schools. In , these children will start turning 65 in large numbers. Many predict that if communities want to be successful in caring for their aging population, they will have to make significant, yet certainly feasible, changes in housing, health care, and human services. In preparing for the needs of large numbers of elderly, it is crucial to think of the challenge as a community issue.
If the care of the elderly begins and ends with entry into a formalized system that takes over when a person is almost unable to function day to day, society will face large service costs and will miss opportunities to help the elderly function as productive, independent citizens for larger portions of their elderly years.
A community's social and economic systems need to become attuned to arranging services to meet the needs of an aging society in natural, informal ways. Most Baby Boomers would like to stay in their own homes, or at least in their own communities, as they age.
Nearly three-quarters of all respondents in a recent AARP survey felt strongly that they want to stay in their current residence as long as possible Bayer and Harper The image that most elders will move to a retirement village away from their communities is the exception rather than the rule. In thinking about community capacity, three stages of community aging can guide planning: Perhaps the most important challenge of the healthy active phase of aging is for a community to learn how to tap the human resources that elders represent in the community.
This is a phase where elders can be key volunteers to improve the life of many segments of a community. Healthy elders can be considered a potential component of the paid workforce if jobs can be structured to meet their changing preferences and capabilities. The second phase of aging, when elders begin to slow down and may face some challenges in doing the every day activities required of community living, represents a subtle challenge for communities. Elders in this phase often need assistance with transportation to remain independent, and communities need to take the lead to develop affordable transportation systems U.
Department of Transportation Safe and affordable housing options also are a priority for community capacity efforts. At this phase of aging, many elders want to move into smaller housing units that are more aging-friendly but still are affordable and integrated in the community. It is important to begin developing such options on a large scale in the coming 10 to 20 years.
In a community with five thousand projected elders, for example, a project with 30 units will not meaningfully attack the problem. Voluntarism is an important community need for elders who are mostly independent but slowing down Butler Volunteers can provide services in a manner that makes elders continue to feel connected to a community and not dependent on a formal care system. And, volunteers often can act as preventive medicine, keeping away the effects of social isolation and keeping elders as active and engaged as possible. Volunteer capacity does not emerge without effort, however.
Communities need to recruit, train, and support volunteers. These caregivers also need support through training programs and respite programs. Many believe that additional financial assistance for family caregivers is needed as well Stone and Keigher Such efforts to support family care-giving also represent an important aspect of community capacity to support elders.
It is unclear whether such local care systems can emerge naturally through market forces or whether market failures will emerge to block the evolution of care systems that reflect the wants and needs of elders. Clearly, the large financing roles of Medicare and Medicaid give the public sector an interest in ensuring that adequate systems of care emerge. How many people will require formal services in ?
As discussed earlier in the paper, this is an unanswerable question in the year If efforts at healthy aging are successful and if informal caregivers and volunteers can help to meet the needs of elders, the total number of frail who need formal services in a community in could be quite similar to the number in , even though the number of elders will more than double.
Keeping the number of frail constant at levels must be the goal of every community to keep costs affordable. However, even if the aggregate number of frail elders stays the same or grows slowly, formal care capacity must be better structured at the community level. Importantly, most communities rely too much on nursing homes as the source of formal care, at least for Tweeners and the Medicaid Bound populations.
Sixty-seven cents of every public dollar supporting long-term care for the elderly is spent on institutional care Congressional Budget Office , despite the clear preferences of frail elders for services in the community. Why does this mismatch of dollars versus preferences happen? The other common forms of exercise for the elderly include stretching rubber bands, performing leg exercises while in bed or sitting in a chair.
The essential function of the lower extremities is to lift our body. If we are not resisting gravity by standing, the crucial elements of physical fitness are at risk of declining. Read more Read less. Kindle Cloud Reader Read instantly in your browser. Product details File Size: Wartooth Ebooks August 3, Publication Date: August 3, Sold by: Share your thoughts with other customers. Write a customer review. Amazon Giveaway allows you to run promotional giveaways in order to create buzz, reward your audience, and attract new followers and customers.
Learn more about Amazon Giveaway. Set up a giveaway. There's a problem loading this menu right now. Learn more about Amazon Prime. Get fast, free shipping with Amazon Prime. Get to Know Us. English Choose a language for shopping. Not Enabled Word Wise: Not Enabled Enhanced Typesetting: Enabled Amazon Best Sellers Rank: Amazon Music Stream millions of songs.
Amazon Advertising Find, attract, and engage customers. Amazon Drive Cloud storage from Amazon. Alexa Actionable Analytics for the Web.