Kingdom Hearts: Birth by Sleep (Video Game ) - IMDb
Edit Cast Cast overview, first billed only: Terra voice Willa Holland Aqua voice Jesse McCartney Master Xehanort voice Haley Joel Osment Master Eraqus voice James Patrick Stuart Braig voice David Dayan Fisher Dilan voice Derek Stephen Prince Even voice David Boat Aeleus voice as Dave Boat Kirk Thornton Isa voice Quinton Flynn Lea voice Richard Epcar Terra-Xehanort voice Luke Manriquez Young Sora voice Ty Panitz Edit Storyline A prequel to Kingdom Hearts the player plays as three different keyblade wielders.
Three friends, three destinies. Everything will link back to the beginning.
Edit Did You Know? Trivia A World based on The Jungle Book , was to appear in this game, but was taken out for timing constraints and similarities to the jungle located in the Neverland Peter Pan World. The World was also supposed to appear in the original Kingdom Hearts , but was taken out there due to similarities to the Deep Jungle Tarzan World.
The World can still be accessed in this game's code in the Japanese Version anyway , with areas such as King Louie's throne room, a mountainside on the way to the Man Village, and a river with giant lily flowers to cross to play in. In this game, we see that it was actually Queen Minnie who ordered Pete's banishment. Seek out the darkness that upsets the balance, and bring an end to him! Health Add to myFT. A Tokyo business is offering to give its workers a bonus if they can prove sufficient bed rest. Leo Lewis November 20, Listen to this article Play audio for this article Pause Explore the Special Report.
About this Special Report. Cookies on FT Sites We use cookies for a number of reasons, such as keeping FT Sites reliable and secure, personalising content and ads, providing social media features and to analyse how our Sites are used. Close Financial Times International Edition. Search the FT Search. World Show more World links.
US Show more US links. Companies Show more Companies links. Markets Show more Markets links. Opinion Show more Opinion links. Conversely, partial night sleep deprivation induced decreases in stimulated production of IL-2 and natural killer cell responses [ 23 , 24 ]. On the PSD-L night, levels of norepinephrine and epinephrine significantly increased in association with nocturnal awakening. Elevated plasma concentrations of C-reactive protein CRP are indicative of systemic inflammation.
Circulating CRP levels are representative marker of vascular damage progression. Additionally, excessive waking periods would induce long-standing psycho-social stress. Recently, stress exposure has been found to lead to increased salt intake and inhibition of renal salt excretion [ 27 ]. These processes may be related to HT development during volume overload for 24 hr and to arterial remodeling.
In short, sleep deprivation is associated with increased sympathetic tone. Sleep loss might serve to elevate nocturnal catecholamine levels and contribute to cardiovascular disease. Short sleep duration imposed on a group of healthy subjects increased sympathetic nervous system activity and blood pressure elevation. Therefore sustained short sleep duration could lead to adverse cardiovascular consequence. A prospective study in the United States showed that the standardized mortality ratio of CHD was highest among those who worked 67 hr or more a week [ 28 ].
Case-control studies in The Netherland [ 29 ], Denmark [ 30 ], and Sweden [ 31 ] also reported that prolonged working time was associated with an increased risk of acute myocardial infarction AMI. Another case-control study in Japan found significantly increased odds ratios of AMI for those who worked more than 11 hr a day [ 32 ].
It is possible to think that sleep deprivation caused by overtime work is associated with an increased risk of AMI. The Alameda County Study [ 10 ] and the study by Partinen et al. In a Japanese case-control study, Liu et al. The cases were men aged admitted to hospitals with AMI during The controls were AMI-free men matched for age and residence who were recruited from the resident registers.
Longer working hours were related to shorter hours of sleep, and more days a week with less than 5 hr in both AMI patients and normal healthy subjects. Working more than 60 hours per week was related to increased incidence of AMI; those working such hours were twice as likely to develop AMI than those working no more than 40 hours. Those who slept no more than 5 hr per night had a 2. A total of coronary events were documented fatal and nonfatal during the 10 years of follow up.
This Japanese company pays its employees to get a good night's sleep
The age-adjusted relative risks of CHD, with 8 hr of daily sleep being considered the reference group, for individuals reporting 5 or fewer, 6, and 7 hr of sleep were 1. The relative risk for 9 or more hr of sleep was 1.
These reports support the notion that short or long sleep duration is independently associated with an increased likelihood of coronary events. There is thus a U-shaped relationship between sleep duration and CHD incidence. Several biological explanations are possible for the increased risk of CHD associated with sleep deprivation.
Hypertension and increased sympathetic nervous system activity may underlie this relationship. Sleep deprivation also increases sympathetic nervous system activity, heart rate, and vasoconstriction as well as salt retention. These factors may be associated with hypertension caused by cardiac overdrive and volume overload. On the other hand, there have been few reports on the relationship between long sleep duration and CHD.
Sleep apnea syndrome would be a candidate factor for this relationship, but there is little evidence as to whether patients with sleep apnea have long sleep duration or not. Lower glucose tolerance, higher evening cortisol concentration, and increased activity of the sympathetic nervous system occurred in the sleep deprivation experiment than in the fully rested condition. Similar results, that sleep deprivation was associated with lower glucose tolerance and increased insulin resistance, were found elsewhere [ 37 ].
Whereas these results were based mainly on an experimental sleep restriction, the metabolic effects of habitual sleep restriction were reported recently. Compared with those sleeping 7 to 8 hr per night, subjects sleeping 5 hr or less and 6 hr per night had adjusted odds ratios of 2. These associations persisted when subjects with insomnia were excluded. The risk elevation remained essentially unchanged after adjustments for age, hypertension, smoking status, self-rated health status, education, and waist circumference.
Short or long sleep duration increases the risks of developing DM, independent of confounding factors. This suggests that U-shaped associations exist between sleep duration and the incidence of DM. Short sleep duration was associated with disruption of endogenous system via increased sympathetic nervous system activity. Several studies have identified some agents that links short sleep duration and incidence of DM. Experimental sleep deprivation causes elevated evening levels of cortisol that may predispose individuals to insulin resistance [ 36 , 40 ].
On the other hand, recent studies have linked sleep disruption with reduced testosterone levels [ 41 ]. Low levels of testosterone have been associated with obesity [ 42 ], elevated levels of insulin and glucose [ 43 , 44 ], and DM incidence [ 45 , 46 ].
In the MMAS [ 39 ], not cortisol but testosterone level had considerable impact on the relationship between sleep duration and DM incidence among male subjects. In addition to this, sleep deprivation reduced levels of leptin and increased levels of ghrelin. Increased appetite was correlated with an increased ratio of ghrelin to leptin [ 47 ]. Sleep restriction results in an increase in sympathetic tone, which inhibits pancreatic function [ 36 , 48 ].
Autonomic nervous system dysregulation may be also associated with the impact of sleep deprivation on the increased incidence of DM. On the other hand, few studies have investigated the effect of long-term sleep duration on triggering DM. Sleep-disordered breathing, a known cause of daytime sleepiness, would be linked to increased sympathetic tone and glucose intolerance [ 7 ].
These mechanisms may be associated with the relationship between long sleep duration and DM. In summary, sleep loss was associated with DM via endocrine system disruption, which would, in part, affect our eating behavior and autonomic balance.
Listen to this article
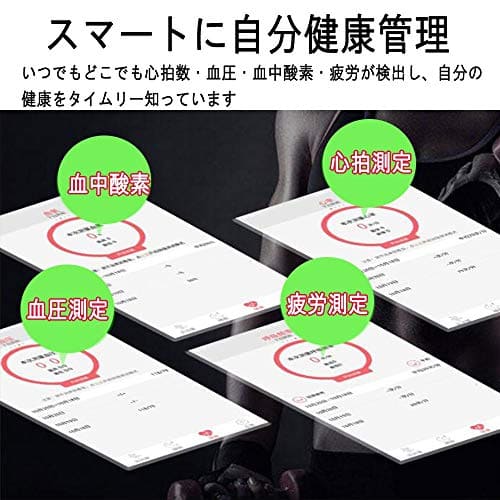
Chart for the relationships between sleep deprivation and hypertension, diabetes mellitus, and coronary heart disease. Recent studies have shown that dysregulation of melatonin secretion may be associated with HT and IGT. The suprachiasmatic nucleus SCN in the hypothalamus, which serves as an essential component of the circadian clock, affects melatonin secretion. Light activates SCN neurons via retino-hypothalamic glutamate secretion.
The SCN reaches autonomic neurons of the paraventricular nucleus PVN which projects to the intermediolateral column of the spinal cord IML where preganglionic sympathetic neurons are located that control the outflow to the pineal gland [ 49 - 51 ]. Injection of transneuronal tracers into various organs ranging from heart to ovaries and from white to brown adipose tissue resulted in the labeling of neurons in the SCN via the sympathetic and parasympathetic branches of the autonomic nervous system [ 55 - 58 ].
These data demonstrate that the SCN may transmit its circadian message, influencing the activity — rest cycle of peripheral organs, not only by the secretion of hormones that may freely pass all kinds of tissue barriers, such as melatonin, corticosterone, gonadal hormones and thyroid hormones but also by direct nervous system control of these organs. And, SCN neurons are labeled via both the sympathetic and parasympathetic systems, indicating that the SCN may indeed support both the activity and rest periods of the circadian cycle.
Sleep Duration as a Risk Factor for Cardiovascular Disease- a Review of the Recent Literature
The SCN-PVN-autonomic axis affects hormone secretion and the sensitivity of the target organs to these hormones through neuronal mechanisms. For example, anatomical and physiological evidence shows that the SCN influences the level of insulin secretion from the pancreas [ 59 - 61 ]. Additionally, when the SCN stimulates glucose secretion from the liver, at the same time it stimulates glucose uptake by other tissues [ 61 ].
This timely orchestrated action of the SCN on glucose metabolism prepares the body, just before waking, for the coming period of activity. Disruption of this orchestration may be associated with the pathophysiology of HT and DM. For a long time, physiological studies have indicated that patients suffering from these diseases exhibit disturbed circadian rhythm [ 62 , 63 ]. Severe decreases in staining for several SCN neurotransmitters in hypertensive patients revealed an anatomical basis for these disturbances [ 64 ].
This intriguing observation suggests that SCN activity is changed by a different autonomic feedback in HT. Furthermore, recent evidence supports the notion that circadian disturbances can be detected before the development of HT or DM [ 65 , 66 ]. In the evening of the day after sleep deprivation, sympathetic nervous system activity and BP are elevated. These increases may be associated with the increased risk of CHD. On the other hand, because sleep deprivation is related to reduced salt excretion or IGT, excessive intake of calories or salt should be avoided by people who are not getting enough sleep.
In addition, since alcohol intake with sleep deprivation tends to elevate BP the next evening, people also should avoid drinking alcohol after not getting enough sleep. However, there is little evidence to support the notion that a sympathetic system blockade could be truly beneficial to such populations. Recently, Scheer et al. Repeated melatonin intake reduced nocturnal systolic and diastolic BP by 6 and 4 mmHg, respectively Fig.
- Navigation menu.
- Sleep Duration as a Risk Factor for Cardiovascular Disease- a Review of the Recent Literature?
- Adventures Of A Waterboy;
- LIVING ABOARD A BOAT NAMED FARFETCHED!
- Beachcombing;
The treatment did not affect heart rate. Repeated but not acute melatonin intake also improved sleep.